

Impaired collagen remodelling following injury is the main contributor for formation of scars. In an scarred tissue organization of collagen fibers is disrupted and there is an imbalance between collagen insertion and removal in the injured skin. The result is too much disorganized fibers, a feature particularly seen in aging acne scars. As we discuss later in the following this disorganization becomes more apparent with aging.
Aging skin appears more thin, smooth, dry with less elasticity and number of pores.
1- Decrease in connective tissue matrix, its fibers, collagen and elastin and its cells, fibroblasts. decrease in GAGs, glycosaminoglycans, which is the main ingredient of connective tissue matrix. GAGs normally bound to associated proteins such as fibronectin and laminin. This binding diminshes substantially in aging. Organization of collagen and elastin fibers is also impaired. This is to a great extent due to breakdown of assoicated protiens. This decrease includes chondritinf sulfate and hyaluronic acid. Hyaluronic acid requires zinc and magnesium for its synthesis. Deficiencies of these elements can results in hyaluronic acid abnormalities, seen in Marfan and Ehler Danlos syndromes. Keratin sulfate increases. Decrease in collagen and elastin could be as a result of either loss of these fibers or a decrease in their production and solubility. The net result is less support for uppermost layer, epidermis. Skin scarring becomes more pronounced. Aging-related atrophy of subcutaneous muscles aggravates the situation.
2- Reactive oxygen species, ROS, generation and direct skin damages due to free radical formation. oxidative stress associated with free radicals can cause lipid peroxidation and cell membrane disruption. this process could be triggered by UV rays as well as aging acne scars. Many lipid soluble vitamins, vitamin C and gluthantione, known antioxidants, may reduce oxidative stress. Reactive oxygen species may directly affect cell organells such as mitochondria and endoplasmic reticulum leading to cellular dysfunctions.
3- Role of cytokines such as interlukin1 and TNF as inflammatory mediators. UV in particular can induce cytokine and growth factors cell surface receptors. These mediators in turn involve in generation of reactive oxygen species which cause collagen destruction and thymine-thymine dimer formation in DNA, more damage to skin connective tissue. Cytokines may directly target type I and type III procollagen and diminish their concentration in extracellular matrix. This result in skin thinning, loss of elasticity and aggravation of skin scars.
4- Chronic high levels of glucose and formation of advanced glycosylation products are among other changes in pathology as a result of skin aging in prolonged untreated acne scars. This leads to cell swelling and disruption of the membrane. Proper glycemic control may delay formation of these molecules and prevent oxidative stress. Growing evidence indicates that severe spikes in postprandial blood sugar care a major problem for non-diabetic as well. Formation of advanced glycation end products and increased generation of free radicals are two main mechanisms by which post-meal hyperglycemia can causes serious aging-related problems such as arterial wall damage.
5- Polyunsaturated fatty acids are a major component of cell membranes and their deterioration can cause interruption in many of the cellular functions.
6- Less blood flow to the skin and decrease in its microcirculation. The skin becomes more susceptible to injury and healing period turns longer.
Impaired collagen remodeling following cutaneous injury is recognized as a primary contributor to scar formation, particularly in individuals predisposed to aberrant wound healing. In scarred skin, the orderly alignment of collagen fibers is significantly disrupted, resulting in a disorganized extracellular matrix (ECM) architecture. This dysregulation reflects a pathological imbalance between collagen synthesis and degradation during the reparative process. The consequence is an excessive accumulation of randomly oriented collagen fibers—a histological hallmark of atrophic and hypertrophic scars, and particularly evident in chronic aging acne scars.
Aging skin is characterized by structural and functional deterioration manifesting as thinning of the dermis, reduction in elasticity, dryness, and a diminished vascular network. These changes are attributed to both intrinsic aging and extrinsic stressors, notably ultraviolet (UV) radiation and environmental pollutants.
One of the most profound changes in aging skin is the decrease in the connective tissue matrix and its key components, including collagen, elastin, fibroblasts, and glycosaminoglycans (GAGs). GAGs such as hyaluronic acid and chondroitin sulfate play a central role in maintaining dermal hydration and ECM integrity. The synthesis of hyaluronic acid, for example, requires trace elements like zinc and magnesium, and deficiencies in these elements have been implicated in disorders such as Ehlers-Danlos Syndrome and Marfan Syndrome, where ECM abnormalities are prominent.
The breakdown of matrix-associated proteins (e.g., fibronectin and laminin) in aging reduces GAG-binding capacity, leading to further deterioration of ECM structure. Notably, keratan sulfate levels may paradoxically increase, although this does not compensate for the loss of hyaluronic acid and chondroitin sulfate.
The cumulative effect is reduced dermal support for the epidermal basement membrane, thereby exacerbating the appearance of pre-existing acne scars and contributing to skin laxity and wrinkle formation.
Oxidative stress plays a pivotal role in the cutaneous aging process. The accumulation of reactive oxygen species (ROS), particularly following UV exposure, leads to lipid peroxidation, protein denaturation, and mitochondrial dysfunction. These processes impair cellular repair mechanisms and accelerate degradation of collagen and elastin fibers.
Antioxidants such as vitamins C and E, glutathione, and coenzyme Q10 may mitigate some of these oxidative effects. However, the chronic presence of ROS in aged or UV-damaged skin continues to drive matrix remodeling in favor of degeneration rather than regeneration.
UV radiation and oxidative stress induce the production of inflammatory cytokines, including interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α). These mediators activate downstream pathways that generate more ROS, inhibit collagen synthesis, and induce DNA damage, such as thymine-thymine dimers. More specifically, they disrupt the transcription of type I and III procollagen, both essential for maintaining tensile strength and resilience of dermal tissues.
Chronic hyperglycemia—even in non-diabetic individuals—facilitates the formation of advanced glycation end products (AGEs). These molecules accumulate in the skin over time and form irreversible crosslinks with proteins, stiffening the ECM and impairing normal cell–matrix interactions. This is particularly concerning in untreated or persistent acne scars, where ECM remodeling is already compromised.
There is a growing body of evidence suggesting that postprandial glucose spikes significantly exacerbate oxidative stress, contributing not only to dermal aging but also to systemic vascular damage.
Polyunsaturated fatty acids (PUFAs) are integral components of cellular membranes. Oxidative damage to these lipids disrupts membrane integrity and impairs a wide range of cellular processes, including signal transduction, ion channel function, and nutrient transport. The resulting membrane dysfunction further hinders the skin’s ability to respond to injury, repair damage, and maintain structural homeostasis.
The interplay between skin aging and acne scarring is complex, multifactorial, and warrants further investigation. While collagen regression with age may, in theory, soften the appearance of dense, fibrotic scars, this potential benefit is often counterbalanced by epidermal thinning, ECM collapse, and loss of dermal elasticity.
Interestingly, some superficial acne scars and post-inflammatory hyperpigmentation may improve with age due to slower melanocyte activity and gradual skin turnover. However, deeper atrophic scars frequently become more visible due to the loss of supportive subcutaneous structures such as adipose tissue and facial muscles.
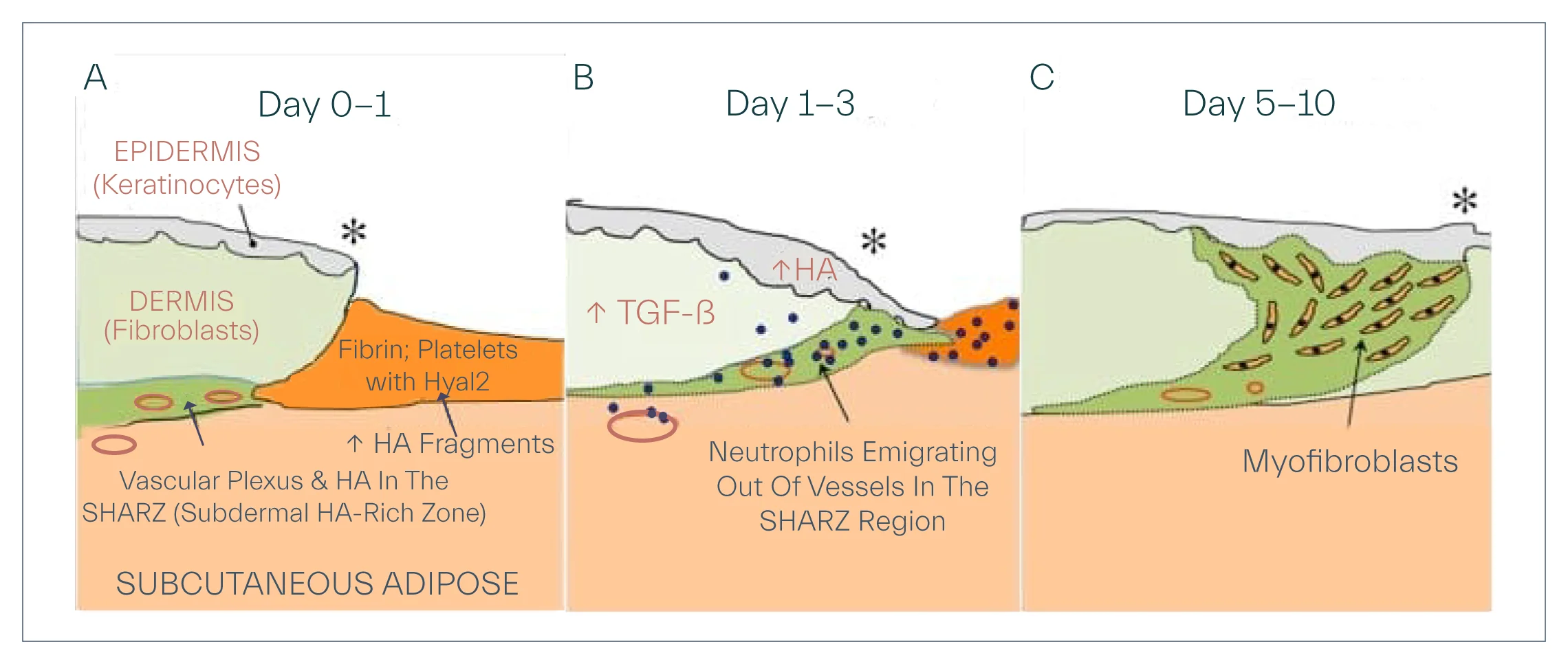
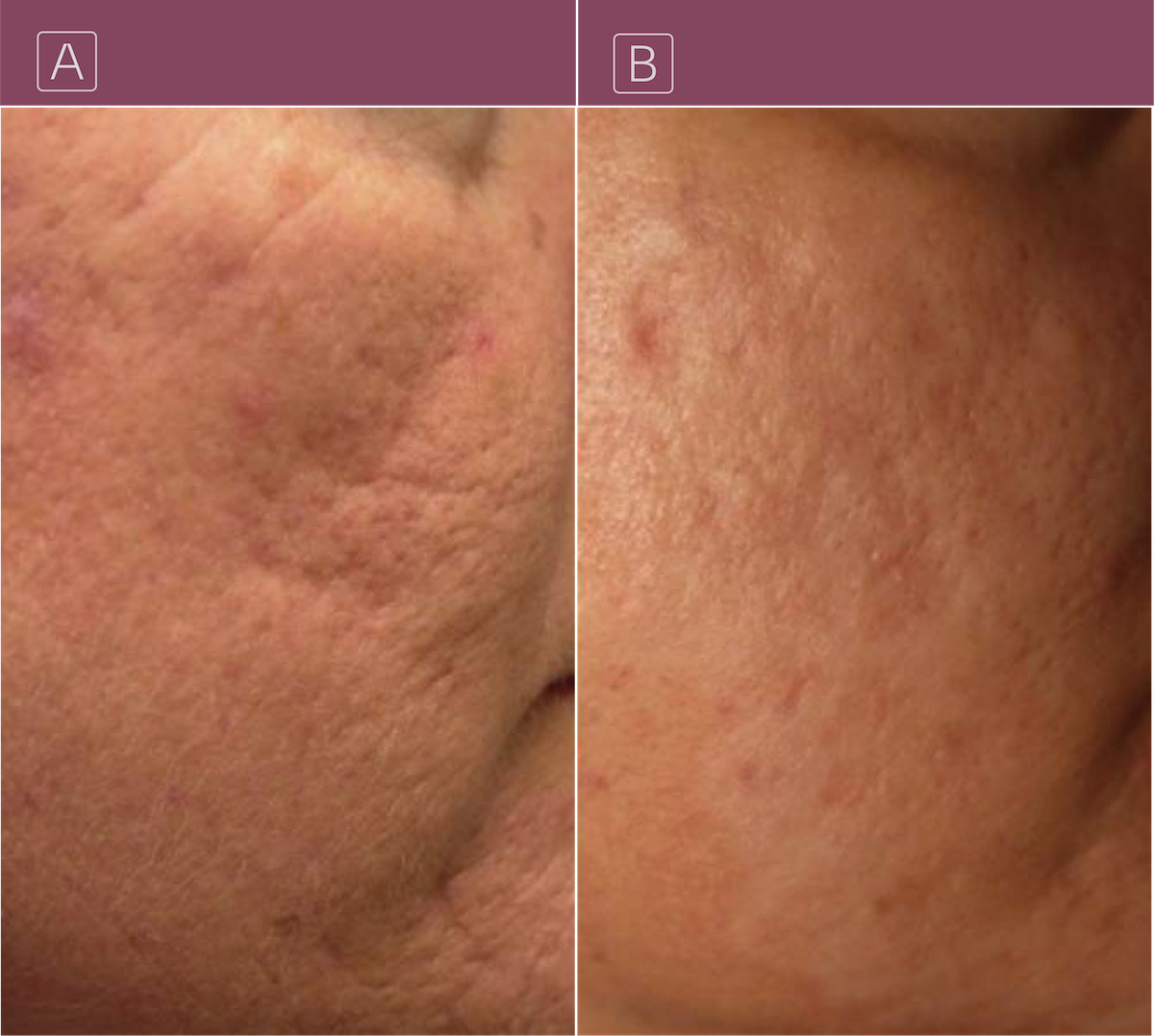
Evidence supports the notion that early therapeutic intervention—particularly resurfacing modalities such as fractional laser therapy, microneedling, and chemical peels—can significantly improve scar appearance and prevent the long-term sequelae of collagen disorganization. These treatments enhance skin texture, tone, and elasticity primarily by stimulating neocollagenesis and improving epidermal barrier function. However, most resurfacing interventions remain superficial, targeting the epidermis and upper dermis without correcting deep ECM abnormalities. A pilot study of 10 patients aged 18 to 60 suggests micronized lipoaspirate injections can increase pappillary and reticular dermis’ collagen within six months of initiating injections. The study did not reveal how broken lipocytes can produce the change in collagen content of dermis layer and why no one or two years follow up of patients was not pursued. While the results seem incipiently encouraging, they insinuate doubt into the outcomes as to whether the observed change in appearance of scars was due to filling effect of injectables or due to a meaningful boost in reticular and papillary collagen.
The aging process exerts a profound impact on the appearance and pathology of acne scars, particularly through mechanisms involving collagen degradation, oxidative stress, and extracellular matrix breakdown. While certain age-related processes may appear to mitigate the rigidity of scar tissue, the overall impact of skin aging tends to exacerbate the visibility and persistence of acne scarring.
How these changes affect aging acne scars requires further investigation and research. Regression in collagen fibers accumulated in scarring seem to lessen the appearance of acne scars, however, decrease in extracellular matrix and its support for epidermis counteract this effect. Scars become more pronounced and may appear as wrinkles. Some shallow acne scars and spots may improve over time. Scar treatment in its early course benefit the patients most by resurfacing the skin and improving its tone and elasticity. Resurfacing treatments do not affect the dermis at a significant level. However, the degree of improvement in overall skin appearance and its tone is substantial.
Given the multifactorial nature of both skin aging and acne scar progression, how might future therapeutic strategies integrate systemic interventions (e.g., antioxidant supplementation, glycemic control) with localized treatments (e.g., ECM-modulating agents, dermal fillers, or stem cell therapies) to provide more holistic and long-lasting results? What role do you foresee for personalized dermatological approaches in managing acne scars across various age groups and skin types?