

Incorporation of essential fatty acids in treatment armamentarium for acne vulgaris has not been standardized yet. However, there are many studies which bring up a possible role for essential fatty acids in treatment of acne and oily skin. Rising antibiotic drug resistance consequent to the widespread use of topical antibiotics and failure of many other topical/systemic treatments in maintenance treatments is causing concern and call for new modalites. Acne is a multifactorial disease and pathologically characterized by increased sebum production which results in an oil forming skin, sebaceous gland hypertrophy, abnormal follicular keratinization and inflammation. Hyperactivity of sebaceous glands may be associated with change in lipid composition of the sebum [1]. This hyperactivity is also a marker of severity of the disease so there is a linear relationship between acne severity and over-secretion of sebaceous glands [2].
There is evidence of association between sebum linoleate concentration and comedo formation. Essential fatty acids deficiency contributes to sebaceous gland hypertrophy and hyperkeratinization of the ducts. Linolenic acid level in the stratum corneum has been reported to be much higher in normal subjects than that in the comedones in particular linoleate content of wax esters. Oily cutaneous and hypersecretion of sebaceous glands is well known as one of four major players in pathogenesis of acne [1] [3]. However, change in composition of the secreted oils during acne has been less studied. Studies by Stewart ME, et al suggest that skin’s fatty acid composition may change with changes in sebaceous gland activity, and that sebum fatty acids can enter the epidermis and be incorporated into epidermal lipids [4]. In this article we are going to examine how different composition of oily secretions in acne patients is from those of normal subjects. We have attempted to look across multiple studies reported in dermatology literature to determine if correction of skin surface lipids can control sebaceous gland overactivity which, in turn, may improve acne.
Studies by Downing et al indicates that differrentiating sebaceous cells implement sebaleic acid instead of linoleic acid in wax esters if the later fatty acid is not available [5]. Sebum fatty acid composition is not fixed but changes in relation to sebum secretion rates. Specifically, with increasing sebum secretion, changes appear to occur both in the lipid class composition (more wax esters compared with cholestrol esters [6] and in the fatty acid composition of the ester lipids [7].
Ceramides, typical structure
Lower amount of sphingolipids and ceramides in keratinocytes of acne subjects of various level of oil level in the skin has been shown [9]. This would be associated in decrease in ability of keratinocytes’ walls to hold water, one possible mechanism that can explain how hyperkeratinization starts in comdeones since impaired water barrier function is concurrently seen in hyperkeratosis. In addition ceramides can trigger nuclear factor-kappa B (NF-kB), leading to induction of human beta defensin-2 (hBD-2) expression, enhancing the skin’s innate antibacterial defense [10].
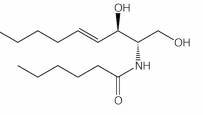
Linoleic acid molecular structure
Although lipogenesis and inflammation are induced by certain propionobactrium acnes strains, sebaceous glands also express proinflammatory cytokines and produce free fatty acids in the absence of bacteria [14]. This may explain a role independent from that of p.acnes for sebaceous gland hyperactivity in pathogenesis of combination skin in acne vulgaris. The same authors [14] suggest generation of antimicrobial peptides by p.acnes in absence of inflammation and proinflammatory cytokines. On the other hand, diets rich in docosahexaenoic acid/eicosapentaenoic acid (DHA/EPA) and gamma-linolenic acid (GLA) have been shown to incorporates metabolites of these fatty acids to epidermal phospholipids, which, in turn, leads to inhibition of leukotriens at the skin level [15].

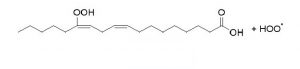
Alpha and gamma linolenic acid follow two pathways in stark distintion
Increase in plasma androgen level induced by steroids cause an increase in cholesterol and free fatty acids in skin surface. Some essential fatty acids such as gamma linolenic acid are potent 5-alpha-reductase inhibitors, suggesting a linkage between unsaturated fatty acids and androgen action [20]. In adult skin androgen action is dependent to conversion of testosterone to five-alpha-dihydrotestosterone. This conversion takes place under enzymatic act of five-alpha-reductase. Cultured sebocytes strongly express 5-alpha-reducatase and 5-alpha-DHT [21]. Hypersensitivity of androgen receptors in pilosebaceous duct and the resulting increase in sebum production and oily skin appears to be associated with a significant increase in free fatty acids rather than other surface skin lipids, a fact that can be incorporated in development of skincare for oily skin.
High skin’s lipid production and the resulting low level of linoleic acid leads to hyperkeratosis, impaired epidermal barrier function and comedo formation. Stimulation of sebocyte proliferation by insulin, thyroid-stimulating hormone and hydrocortisone indicates that the hormonal control of the sebaceous gland is a complex mechanism [21]. Can providing the skin with essential linoleates prevent comedo formation and aid excessively-oil-forming skin to manage itself? A study reports that stratum corneum sphingolipids of adult acne patients is lower than that in control subjects. Decrease in sphingolipids content of cell walls contributes to diminished water barrier function which, in turn, leads to increased permeability to inflammatory substances and comedo formation . All these studies support use of unsaturated fatty acids in treatment of oily skin in acne vulgaris and call for a campaign against long-been-supported and conventionally-recommended oil-free products for oily skin and acne patients by physicians.
Our hypothetical idea is that hypersensitive overworked sebaceous glands in an acne patient do not operate to produce their high-end products such as linoleates, rather, their overflow is associated with cheap secretions from less-differentiated sebocytes such as free fatty acids. There is an inverse relationship between secretion rates and the linoleate content of the surface wax esters. The question that whether local supply of essential fatty acids down regulate the overworked sebaceous glands is supported by studies of Letawe C, et al. Topical application of linoleic acid resulted in significant decrease in size of follicular casts and microcomedones and may be principally used in skin care routine for oily skin[22]. Another study by Charakida ,et al indicates 53% in sebum production and significant improvement in lesions assessed by Leeds acne grading system by using ethyl linoleate for 4 weeks [23]. Moreover, linoleic acid significantly decreases phagocytosis and reactive oxygen species generated by neutrophils [24]. Thus, a practical role for lipid dysregulation in acne pathogenesis and its correction stays a demanding area for research in treatment and regulation of squalene peroxidation generated by neutrophils gland hyperactivity.
The therapeutic potential of essential fatty acids (EFAs) in the management of acne vulgaris and oily skin represents a promising but underexplored avenue in dermatological research. While acne remains a multifactorial dermatosis characterized by hyperseborrhea, follicular hyperkeratinization, inflammation, and Cutibacterium acnes colonization, emerging evidence underscores the role of skin surface lipid composition—particularly EFA deficiency—as a key pathogenic contributor. Despite the well-documented overproduction of sebum in acneic skin, a nuanced understanding of qualitative alterations in sebum lipid profiles remains limited. The incorporation of EFAs into acne treatment regimens is not yet standardized, yet current literature increasingly supports their role in modulating sebaceous gland activity and restoring cutaneous homeostasis.
A pivotal element in acne pathophysiology is the altered sebaceous lipid profile, particularly the diminished levels of linoleic acid within comedonal follicles. This deficiency may lead to sebaceous gland hypertrophy and contribute to aberrant follicular keratinization, forming a conducive environment for comedone development. Studies such as those by Downing et al. illustrate a compensatory substitution of sebaleic acid for linoleic acid in wax esters, indicating the plasticity of sebaceous gland lipid synthesis in response to substrate availability. This biochemical adaptability underscores the need to re-evaluate traditional acne treatments by considering nutritional and topical replenishment of linoleic acid.
In addition to structural lipid changes, the impact of linoleic acid deficiency on epidermal sphingolipids, particularly acylceramides, further exacerbates barrier dysfunction and inflammation. Dysfunctional ceramides compromise the stratum corneum’s water retention capacity, potentially initiating hyperkeratosis through epidermal dehydration and impaired desquamation. This pathophysiological sequence aligns with observations of decreased ceramide content in acne-prone skin, offering a mechanistic explanation for follicular plugging in comedo formation.
Interestingly, the sebaceous gland’s proinflammatory role independent of C. acnes colonization adds further complexity to acne pathogenesis. Inflammatory mediators, including free fatty acids and cytokines produced by sebocytes, may sustain cutaneous inflammation even in the absence of microbial triggers. This finding aligns with research indicating that endogenous lipogenesis in sebaceous glands is sufficient to provoke inflammatory cascades, underscoring the relevance of targeting sebocyte metabolism directly.
Moreover, unsaturated fatty acids such as alpha-linolenic acid (ALA), docosahexaenoic acid (DHA), and gamma-linolenic acid (GLA) have demonstrated the ability to modulate sebum production and inflammatory signaling. These EFAs appear to attenuate NF-κB-mediated inflammation via activation of peroxisome proliferator-activated receptor gamma (PPAR-γ), a nuclear receptor implicated in lipid metabolism, sebocyte differentiation, and immune regulation. Activation of PPAR-γ promotes terminal sebocyte differentiation, thus offering a dual-action benefit by reducing both lipid hypersecretion and proinflammatory cytokine expression.
Further reinforcing this therapeutic potential is the observation that GLA inhibits 5α-reductase, the enzyme catalyzing the conversion of testosterone to dihydrotestosterone (DHT), a potent stimulator of sebaceous gland activity. Given the androgen dependence of sebaceous gland function, EFAs with anti-androgenic properties offer a biochemically rational intervention for oily skin and hormonally mediated acne.
Lastly, the oxidative susceptibility of squalene—a major component of sebum—presents another target for intervention. Upon exposure to UV radiation, squalene undergoes peroxidation, yielding by-products that exhibit comedogenic and cytotoxic properties. This oxidative damage may amplify both inflammatory and hyperkeratotic pathways in acne pathogenesis. Incorporating EFAs with antioxidant properties or those that modulate lipid composition may limit squalene oxidation and its downstream pathological effects, further supporting the rationale for EFA supplementation.
Taken together, these findings suggest that correcting skin lipid imbalances through essential fatty acid supplementation—whether dietary or topical—may constitute a novel adjunctive strategy for managing acne vulgaris and oily skin. Targeting the sebaceous gland’s lipid output and inflammatory potential through modulation of fatty acid composition could offer a mechanistically sound and non-antibiotic therapeutic approach. Future clinical studies are warranted to standardize dosages, formulations, and delivery mechanisms, thereby facilitating the integration of EFAs into evidence-based dermatologic practice.
Stimulatory effect of androgens on sebocytes has been well known in vitro and in vivo. However, various species of androgens function differently on sebcacous glands locationwise. Facial sebocytes are under influence of testosterone and dihydrotestosterone (DHT) with later having the strongest effect while body sebocytes are up regulated by dihydrotestosterone (DHT) and their proliferation affected negatively by testosterone [25]. Inhibitory effect of acylceramide with linoleic acid on keratinocytes hyperplasia induced by UVB exposure [26].
1. Harris HH, Downing DT, et al.
Sustainable rates of sebum secretion in acne patients and matched normal control subjects. J American Academy of Dermatology. 1983;8(2):200-203.
2. Cunliffe WU, Dunitz M. In: Acne. 1989.
3. Pierard-Franchimont C, Pierard GE, et al. Comparison of the kinetics of sebum secretion in young women with and without acne. Dermatologica. 1991;183(2):120-122.
4. Stewart ME, Grahek MW, Wertz WW, et al.
Dilutional effect of increased sebaceous gland activity on the poroportion of linoneic acid in sebaceous wax esters and in epidermal acylceramides. J Invest Dermatol. 1986;87(6):733-6.
5. Downing DT, Strauss JS, et al. Essential fatty acids and acne. J Am Acad Dermatol. 1986;14(2 Pt 1):221-5
6. Downing DT, Stewart ME. Meseaurement of sebum secretion rates in young children. J Invest Dermatol. 1985;84:59-61.
7. Stewart ME, Quinn MA, et al.
Variability in the fatty acid composition of wax esters from vernix caseosa and its possible relation to sebaceious gland activity. J Invest Dermatol. 1982;78:291-295.
8. Matoltsy AG. Keratinization. J Invest Dermatol. 1976;67:20-25.
9. Yamamoto A, Takenouchi K, Ito M. Impaired water barrier function in acne vulgaris. Arch Dermatol Res. 1995;287(2):214-8.
10. Schutze S, Pottoff K, Machleidt T, et al.
TNF activates NF-kappa B by phosphatidylcholine-specific phspholipase C-inuced acidic shingomyelin breakdown. Cell. 1992;71(5):765-76.
11. Summerly R, Yardley H J, Raymond M, et al. The lipid composition of sebaceous glands as a reflection of gland size. Brit J Dermatol. 1976;94(1):45-53.
12. Chiba K, Yoshizawa K, et al. Comdeogenicity of squalene monohydroperoxide in the skin after topical application. J Toxicol Sci. 2000;25(2):77-83.
13. Picardo M. Zompetta C, De Luca C, et al. Role of skin surface lipids in UV-induced epidermal cell changes. Arch Dermatol Res. 1991;283:191-197.
14. Zouboulis CC. Propionibacterium acnes and sebaceous lipogenesis: A love-hate relationship? J Invest Dermatol. 2009;129:2093-2096.
15. Miller CC, Tang W, Ziboh VA, Fletcher MP.
Dietrary supplementation with ethyl ester concertates of fish oil (n-3) and borage oil (n-6) polyunsatrated fatty acids induces epidermal generatio of local putative anti-inflammatory metabolites. J Invest Dermatol. 1991;86(1):98-103.
16 Strauss JS, Pochi PE, whitman EN. Suppression of sebaceous gland activity with Eicos-5:8:11:14-Tetraynoic acid. J Invest Dermatol. 1967;48(5):492-493.
17. Clarke BA, Clark DC.
Suppression of rat liver fatty acid synthesis by Eicosa-5,8,11,14-tetraynoic acid without a reduction in lipogenic
enzymes. J Nutr. 1982;112:1212-1219.
18. Zhao G, Etherton TD, Martin KR et al. Anti-inflammatory effects of polyunsaturated fatty acids in THP-1 cells. Biochem Biophys Res commun. 2005;113:1011-1020.
19. Zouboulis CC. Acne and sebaceous gland function. Clin Dermatol. 2004;22(5):360-6.
20. Liao S. Androgen action: molecular mechanism and medical application. J Formos Med Assoc. 1994;93(9):741-51.
21. Zouboulis CC, Seltmann H, Fritsch M, et al.
The human sebocyte culture model provides new insights into development and management of seborrhea and acne. Dermatology. 1998;196(1):21-31.
22. Detawe C, Boone M, Pierard GE.
Digital image analysis of effect of topically applied linoleic acid on acne microcomedones. Clin Exp Dermatol. 1998;23(2);56-8.
23. Charakida A. Chu AC, et al.
Double-blind, randomized, palcebo-controlled study of a lotion containing triethyl citrate and ethyl linoleate in the treatment of acne vulgaris. BR J Dermatol. 2010;163(2):437.
24. Akamatsu H, Komura J, Miyachi Y, et al. Suppressive effects of linoleic acid on neutrophil oxygen metabolism and phagocytosis. J invest Dermatol. 1990;95(3):271-4.
25. Akamatsu H, zoubooulis CC, Orfanos CE.
Control of human seobocyte proliferation in vitro by testosterone and 5-alpha-dihydrotestosterone is dependent on the localization of the sebaceous glands. J Invest Dermatol. 1992;99(4):509-511
26. Imokawa G, Yada Y, Kawamata A, et al.
Peudo-acylceramide with linoleic acid produces selective recovery of diminished cutaneous barrier function in essential fatty acid deficient rats and has an inhibitory effect on epidermal hyperplasia. J Clin Invest. 1994;94(1):89-96.
* Lovaszi. M, Sebaceous immunobiology is orchestrated by sebum lipids. Dermatoendocrinol, 2017 Oct 17;9(1)