

Cystic acne presents a severe from of acne vulgaris and requires professional advice from a physician. They are rarely cancerous but addition of inflammation and bacteria through their rupture into the skin can render them painful and pus-discharging. Occasionally bacteria enter the cyst and cause an infection which resembles a boil. cysts are more likely to be associated with sequels and acne scars.
Severe cystic forms of acne may be manifestation of a systemic disease such as androgen excess and hormonal imbalance as in polycystic ovarian syndrome and warrants further medical investigation. It is of note that acne conglobata which presents with nodules and interconected cystic lesions with sinus tract, affecting trunk and limbs, is considered a severe and rare form of cystic acne.
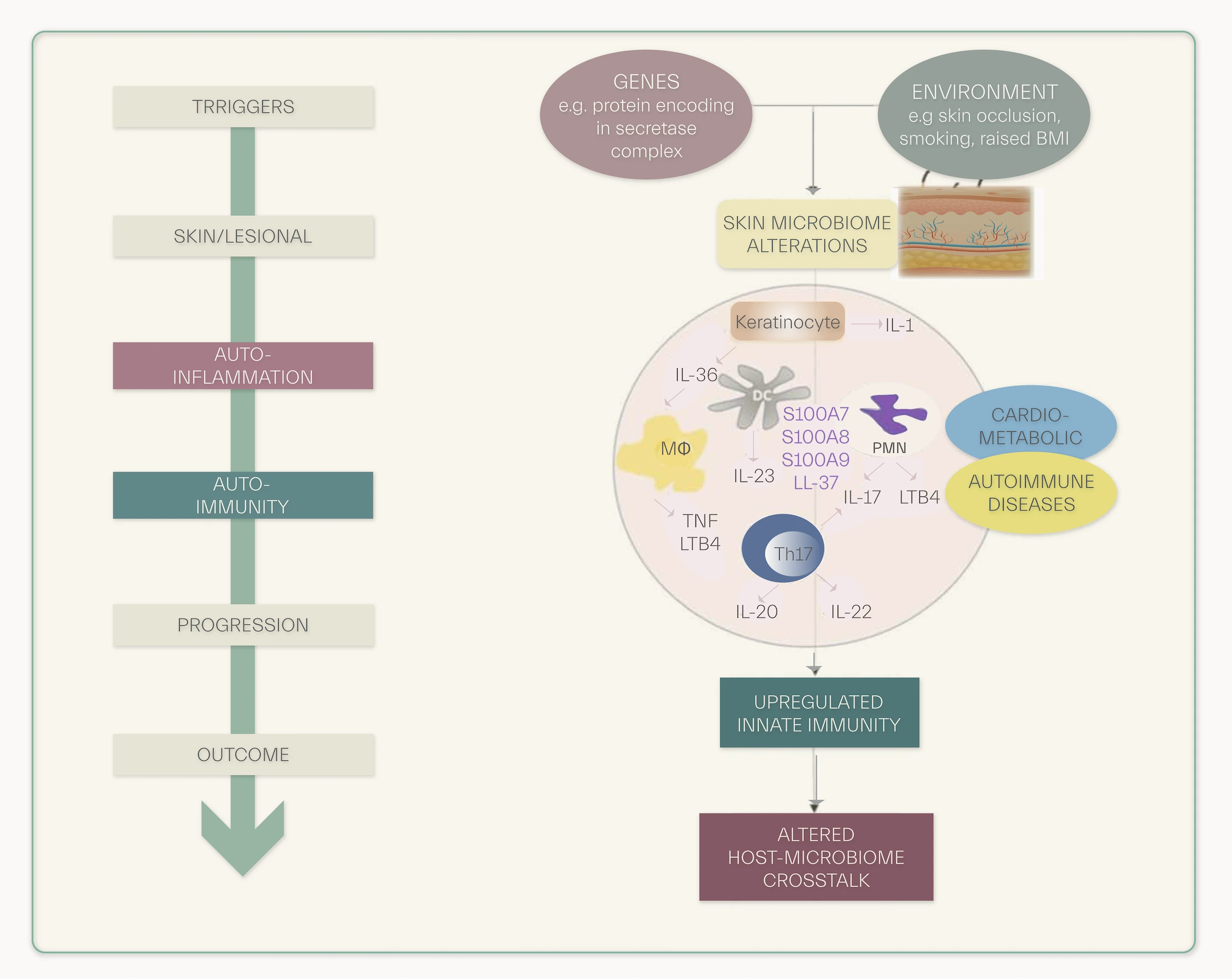
In its differential diagnosis hidradenitis supurrative or acne inversa manifested with cysts and nodules on the body with sinus tract, may be considered. Acne inversa in its presentation and pathogenesis differs from acne vulgaris while proinflammatory cytokines are preeminently create a breeding ground for its development. Bacterial resistance to certain antibiotics and disruption of the skin microbiome are among other considerations in evaluating patients with severe acne.
Cystic acne should be consulted with a dermatologist. Small non-acneous cysts don’t usually require systemic treatment, but can be readily removed by a minor surgical procedure or managed using topical acne treatments. Larger ones are usually removed because they are unsightly or because they have been inflamed or can be medically managed.
Cysts are treated by making an excision in the skin. It is usually treated with isotretinoin and oral antibiotic, however, topical treatments may also be beneficial and sufficient in particular when body acne is not existent or considerable or may be used in conjunction with systemic treatment.
Some studies suggest use of carbon dioxide laser treatments combined with topical treatments for this type of acne to avoid systemic treatments and their adverse effects. Photodynamic therapy, PHT, has also been subject of multitude of studies which suggest PHT efficacy in treatment of mild to severe forms of acne. Moreover, cysts are more prone to development of acne sequels. Recurrence is not infrequent especially in case of initial treatment with isotretinoin.

Manifestation of cystic acne
Nonpharmacologic treatments include: Gentle face washing, avoidance of manipulation of acne lesions. Oil-free products do not necessarily provide benefit and may stimulate further sebaceous secretions. Hypersecretion of sebaceous glands and sebum dysfunction in acne subjects render the skin depleted in essential fatty acids, which in turn further change acne microenvironment and result in a redundant excitement of sebaceous glands to produce sebum in excess .
PH-balanced cleansers containing essential fatty acids may correct this deleterious event. Salicylic acid preparations have been found helpful. Evidence-based skin care has gained a substantial role in management of mild to moderate acne as well as maintenance treatment of severe form of acne vulgaris.
Begin remedying with benzoyl peroxide gel in the morning. Add topical tretinoin or Adapalene in the evening. Add topical antibiotic such as erythromycin/clindamycin if not responsive to previous steps. Add systemic antibiotics such as tetracyclin, doxycycline, clindamycin, erythromyin.
If this form of acne is diagnosed, aforementioned steps could be circumvented and systemic agents such as oral isotretinoin can be directly initiated. This agent is associated with serious, dose dependent side effects which should be discussed in details with each patient in an effort to make a shared decision making. Combination therapy with benzoyl peroxide, doxycylcine and adapalen has been proposed to be superior to oral isotretinoin.
While above steps are taken during exacerbation of acne, topical treatment and evidence based acne skin care regimens find their significance in maintenance treatment armamentarium of this severe manifestation of acne. Acne skin care may be used initially in conjunction with oral therapy for optimal result and to avoid certain side effects associated with oral medications such as dry skin and atopic dermatitis. Topical therapy with oil free products may not be advisable as change in skin lipid composition occurs during the course of acne and should be addressed with proper skin care which provide to the skin essential fatty acids.
Cystic acne, a severe manifestation of acne vulgaris, is typified by the formation of deep, inflamed, pus-filled lesions that often culminate in acne scarring. This subtype of acne is characterized by the rupture of sebaceous cysts into the dermis, initiating a cascade of inflammatory and infectious complications. While rarely malignant, these lesions may become secondarily infected by bacterial infiltration, leading to presentations that mimic cutaneous abscesses or boil-like nodules. As such, painful cystic acne with purulent discharge should be managed with urgency to mitigate the risk of post-inflammatory hyperpigmentation (PIH) and atrophic acne scars.
A particularly virulent form of cystic acne is acne conglobata, often considered the most severe phenotype of nodulocystic acne vulgaris. Clinically, it presents with interconnected nodules, cysts, abscesses, and sinus tracts, commonly involving the trunk, shoulders, and upper arms. It is associated with macrocomedones—large, grouped blackheads—and profound inflammatory response, often culminating in keloid or hypertrophic scarring. Early diagnosis and prompt combination antibiotic therapy for severe acne conglobata are essential, frequently necessitating the inclusion of systemic isotretinoin in therapeutic regimens.
Non-pharmacologic measures serve as foundational adjuncts in the holistic management of nodulocystic acne. These include:
Of note, recent dermatological research suggests that patients with moderate to severe acne exhibit sebaceous gland dysregulation and altered skin lipid composition, particularly a deficiency in essential fatty acids. This imbalance creates a pro-inflammatory skin microenvironment, further aggravating sebaceous activity and acne pathogenesis.
The first-line pharmacologic approach to treating cystic acne typically includes a multi-step regimen:
In cases of severe nodulocystic acne, it is often clinically justified to bypass initial topical therapies and initiate oral isotretinoin as first-line treatment. This decision, however, mandates a detailed discussion regarding isotretinoin-related adverse effects, which include mucocutaneous dryness, teratogenicity, and mood alterations. Shared decision-making in isotretinoin therapy is a critical component of patient-centered acne management.
Interestingly, a growing body of literature supports the synergistic efficacy of combination therapy with benzoyl peroxide, doxycycline, and adapalene, which may in some cases offer outcomes comparable or superior to monotherapy with isotretinoin.
Once active inflammation subsides, maintenance therapy for cystic acne is crucial to reduce recurrence and mitigate the need for repeat systemic interventions. This typically involves:
Further, hormonal evaluation in women with persistent cystic acne is warranted, particularly when clinical features suggest androgen excess or polycystic ovarian syndrome (PCOS). In such instances, endocrine therapy (e.g., oral contraceptives or anti-androgens) may be necessary adjuncts.
The differential diagnosis of nodulocystic acne on the trunk and buttocks must include hidradenitis suppurativa (acne inversa)—a chronic inflammatory condition characterized by nodules, abscesses, and sinus tract formation in intertriginous areas. Unlike acne vulgaris, hidradenitis suppurativa pathophysiology is centered on follicular occlusion and dysregulated innate immunity, rather than sebaceous hyperactivity.
Evaluation should also include a review of antibiotic resistance patterns and the impact of prolonged antibiotic therapy on the cutaneous microbiome, as both may influence treatment efficacy and long-term outcomes.
Dermatologic consultation is imperative for the comprehensive management of nodulocystic acne, especially in cases unresponsive to conventional therapy. Treatment options include:
Minor surgical excision of inflamed cysts
These modalities offer the benefit of targeted lesion reduction while minimizing systemic exposure. However, access, cost, and long-term efficacy remain subjects of ongoing research.
Nodulocystic acne vulgaris, particularly in its most severe forms such as acne conglobata, represents a challenging dermatologic condition with significant physical and psychosocial morbidity. A multi-pronged approach involving topical agents, systemic therapy, lifestyle modifications, and professional dermatologic interventions offers the highest likelihood of sustained remission. The emphasis on long-term maintenance therapy for severe cystic acne, coupled with personalized treatment planning, underscores the need for early and consistent engagement with dermatologic care.