

There is no single best mode for management of all acne lesions . Control of different forms is determined by many factors, including types of lesions present, duration of disease, past and present response to modalities, tendency for scarring and development of spots. Knowing the symptoms and early intervention are the key to a successful management. Cystic acne may be hormonally mediated from within and without the skin, which involves in dynamic generation of androgens and imparts a conceding aspect to cystic acne treatment.
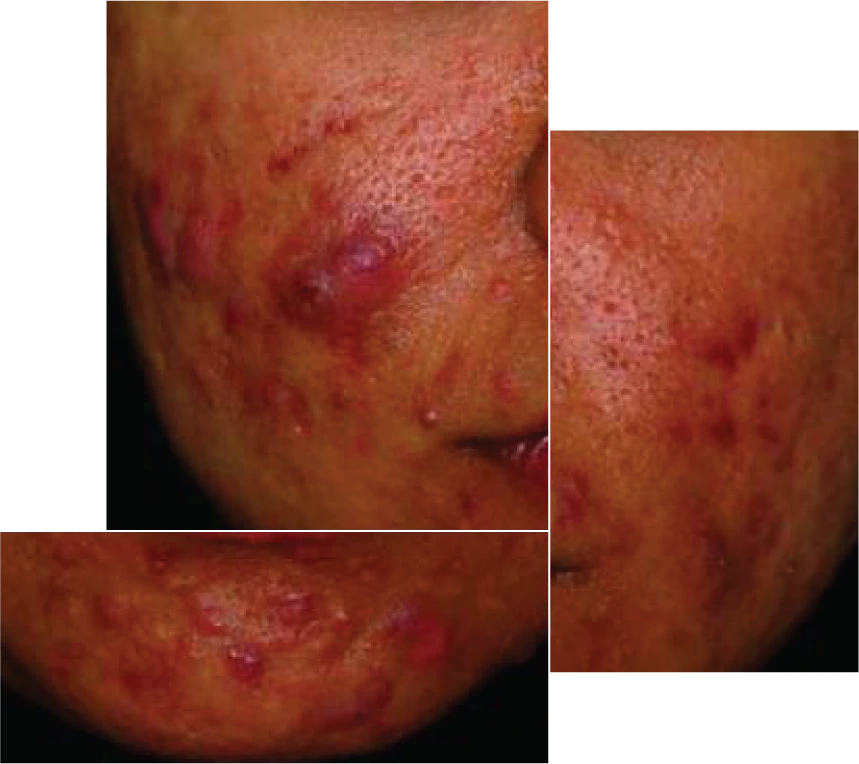
Severe acne is presented with cysts and nodules, scarring and skin discolorations are evident
Cysts and nodules especially when multiple are indicative of severe form of acne and warrant combination therapy with topical and oral agents including topical retinoids and oral antibiotics. Benzoyl peroxide may be used with this regimen, however, its use with topical retinoids is generally too drying and irritating to the skin. This is where acne skin care is substantiated and its practice in maintenance treatment of acne vulgaris, prominently a chronic disease, grow significant. Harsh skin care has been recognized as one of the aggravating factors in acne disease. Oral isotretinoin may be used in recalcitrant cystic acne not responding to other modalities in selected patients. This agent should not be resourced as a first line agent in moderate to severe acne not responding to first round of treatment and caution is exercised for its grave side effect profile.

Comedonal acne, initial stage of acne vulgaris
It is important to note that severe form as in cystic form may warrant combination therapy and must be consulted with a physician. Best approach for mild forms such as comedones (whiteheads and blackheads), small pustules and scattered papules are various treatment modalities with desquamating agents such as benzoyl peroxide. Among leading over-the-counter treatments benzoyl peroxide could be counted. Its antibacterial efficacy is noteworthy in rapid destruction of Porpionibacterium acnes. This suppressive effect is much faster compare with that of antibiotics. In contrast to antibiotics, resident organisms do not become resistant to this agent. This agent also demonstrates anti-inflammatory effect due to a reduction of oxygen free radicals. Its comedolytic effect is comparatively slight in contrast to other topical agents used to treat acne. Contact allergy is quite rare with it.
A comedolytic over-the-counter such as salicylic acid (a beta hydroxy acid), which could be used as alternative or adjunct to benzoyl peroxide in cystic acne treatment. This combination therapy for acne maybe among modalities for moderate forms and may be equally used as most effective cystic acne treatment between the flares. Salicylic acid comedolytic activity justifies its therapeutic value. Keratolytic activity of this BHA causes peeling and removal of top layer of the skin. This can result in preventing the follicles from getting plugged.
Salicylic acid is also moderately effective in destructing Porpionibacterium and shows moderate antibacterial efficacy. Combination therapy of salicylic acid with benzoyl peorxide have been postulated by a more recent study as effective in cystic acne treatment. Application of AHA’s (alpha hydroxy acids) such as glycolic acid may resolve the comedones and prevent more severe form. Use of alpha hydroxy acids alone is not indicated. However, a positive effect through control of sebum production and ductal hypercornification is likely.
Tretinoin in its oral form, isotretinoin is used in refractory cases for cystic acne treatment. Its adverse effects, most commonly skin xerosis and cheilitis mostly induced through apoptosis, should be discussed and may not be sought as an initial rescue.Topical forms is used for managing acne in its mild to moderate forms as well as as adjunct with oral treatments in severe forms of acne. Maintenance therapy between flares of acne and at home regimens is another aspect of a comprehensive treatment to prevent relapses of cystic acne. Treatment of acne vulgaris during pregnancy warrants certain considerations and more specific treatment protocol.
Guidelines of care aids us to treat according to more conventional methods yet more evidence based medicine suggest alternative approaches with a focus more reverent to the skin native microbiome and lipids. Preservation of skin’s own microbiome and avoidance of aggressive use of antibiotics gain more traction in recent literature and call for review of acne treatment guidelines. Natural lipids with antibacterial properties which have been avoided for more than two decades in the guidelines are now focus of attention of multitude of studies on cystic acne treatment. Herbs and naturally-derived preparations may become more studied and recognized in future acne armamentarium. Lately, diet has gained far greater acknowledgement and relevant dietary precautions have been introduced in management of acne vulgaris as it is a chronic ailment and its maintenance as in at home cystic acne treatment in the form of diet, skin care, topical treatments is substantiated.
There exists no universal or singularly optimal strategy for the management of all acne lesions. The therapeutic approach must be tailored to individual patient profiles and influenced by a confluence of clinical factors, including the types of lesions present, disease chronicity, history of therapeutic response, scarring propensity, and pigmentation sequelae. Early recognition of symptoms and timely intervention remain critical pillars in optimizing clinical outcomes, particularly in the management of cystic acne—a severe and often recalcitrant form of acne vulgaris. The hormonal milieu, both cutaneous and systemic, plays a decisive role in the pathogenesis of cystic acne through dynamic androgen synthesis, which underscores the complexity and necessity for individualized treatment paradigms.
A comprehensive patient assessment is imperative when formulating a treatment strategy for cystic acne. This includes evaluation of the current medical status, underlying comorbidities, and medication history—particularly with respect to corticosteroids, oral contraceptives, and long-term topical antibiotic use. Notably, cystic acne may manifest as a dermatologic feature of systemic conditions such as polycystic ovarian syndrome (PCOS) or other forms of androgen excess, necessitating further endocrinologic evaluation.
Psychosocial factors are equally consequential, as stress-related acne exhibits chronicity often resistant to conventional regimens. Personal hygiene practices, cosmetic use, facial care routines, and hair grooming habits must also be scrutinized. Patients should be advised on the expected timeline for therapeutic effect—typically six to eight weeks—and informed that truncal lesions, particularly on the back and chest, often demonstrate slower response rates compared to facial lesions.
The propensity for mechanical manipulation of lesions to exacerbate disease severity and promote scarring must be emphasized during patient education. In the presence of multiple nodules or cysts, a combination regimen involving both topical and systemic agents—most commonly topical retinoids and oral antibiotics—is often indicated. While benzoyl peroxide remains a mainstay of therapy for its potent antimicrobial and anti-inflammatory properties, its concurrent use with topical retinoids can result in excessive cutaneous irritation, necessitating an integrative skin care regimen.
Topical keratolytics and desquamating agents, such as benzoyl peroxide, continue to serve as first-line interventions in comedonal and mild inflammatory acne. Its ability to rapidly reduce Cutibacterium acnes (formerly Propionibacterium acnes) populations without fostering microbial resistance remains its principal advantage. However, its comedolytic potential is modest in comparison to other agents. Salicylic acid, a beta hydroxy acid (BHA), offers complementary action through follicular desquamation and moderate antibacterial activity, making it suitable as either monotherapy or an adjunct to benzoyl peroxide.
Emerging literature supports the combined use of benzoyl peroxide and salicylic acid as a viable regimen for the treatment of moderate to severe inflammatory acne, including cystic variants. Likewise, alpha hydroxy acids (AHAs) such as glycolic acid demonstrate utility in mitigating hyperkeratinization and maintaining follicular patency, although they are not indicated as standalone therapies for moderate or severe disease.
Tretinoin, in both topical and systemic forms, remains central to acne management. While oral isotretinoin is reserved for refractory or severe nodulocystic acne, its adverse effect profile—including cheilitis, xerosis, and potential teratogenicity—necessitates cautious use and should not be prematurely introduced as a first-line agent. Topical retinoids, by contrast, are appropriate in both monotherapy for mild disease and as adjunctive treatment in more extensive cases. Their role in maintenance therapy to prevent relapse is increasingly emphasized.
Conventional guidelines for acne management are progressively being reevaluated in light of growing interest in preserving the skin’s native microbiome and lipid integrity. The indiscriminate use of systemic antibiotics has drawn criticism due to concerns over microbial resistance and disruption of the skin’s protective ecosystem. Accordingly, emerging therapies now explore the utility of naturally occurring lipids and phytochemical compounds with antibacterial properties.
Dietary modulation has also gained prominence in acne research, with growing evidence linking high-glycemic diets and dairy intake to acne exacerbations. This shift encourages incorporation of nutritional counseling into acne management plans, particularly for chronic forms such as cystic acne.
Long-term management of cystic acne necessitates a structured maintenance protocol aimed at preventing recurrence and mitigating complications. An effective topical regimen should target the multifactorial pathogenesis of acne by: (1) preventing comedogenesis, (2) reducing sebum production, (3) minimizing comedonal rupture, (4) resolving and controlling inflammation, and (5) preventing post-inflammatory scarring. The treatment of acne sequelae, especially scarring, remains a substantial clinical challenge and underscores the importance of early and appropriate intervention.